 04.03.2023
04.03.2023
Self-Monitoring. Self-diagnostics. Nuances
BCC
The doctor's office is equipped with all the latest and most advanced equipment to correctly interpret what we see and make the right diagnosis, and ultrasound skin scanning, optical coherence tomography, and laser confocal scanning microscopy. But this will only be done after the patient, the skin tumor mass is well visualized, has reached a certain stage of progression, and may already present histologic, and physiologic problems, and danger. The average person only has the ability to visually assess the condition of his skin, and an attempt to give a proper assessment of what he sees, and this may be quite enough to prevent many disasters.
In this article, we have decided to address only the nuances and problems of self-assessment of the condition of the skin prior to visiting a doctor. To a certain extent, we believe it is necessary to increase oncological caution of ordinary people, due to the alarming epidemiological situation in many countries concerning precancerous and malignant skin formations. We hope that our reader will increase his or her outlook and understanding of which skin growths should be treated with extreme caution, and which skin growths can be dangerous and require urgent and prompt treatment. It is important that in everyday life people can easily notice abnormal skin changes and be promptly diagnosed and treated. Regular skin self-examination is important and should be performed regularly. This makes it possible to detect pathological changes in the skin at the earliest stages and almost guarantees a positive resolution of any malignant pathology.
In this article, we present only a small part of the great variety of external manifestations of skin pathologies that, in our opinion, require commentary and accessible explanation 

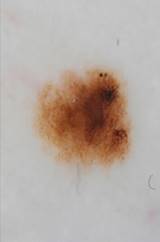
Photo 1 Photo 2
Photos 1 and 2 show the most common basal cell skin tumors (BCC). Progressive stage of nodular BCC. Progression is indicated by the beginning of ulceration, bleeding, and deepening in the center of the tumor mass. Typical teardrop-shaped, slightly pearly or pearl-shaped protruding tubercles on the skin are very often present around the circumference and edges of the tumor. Crater-like ulceration indicates tumor progression and probable even deeper vertical invasion into the tissue.
 Photo 3
Photo 3
In Photo 3, BCC. It is important to note that on absolutely all BCC tumors one can see typical, in large numbers, thread-like, actively growing vessels penetrating the tumor. This is a characteristic diagnostic sign. This is because the tumor produces an abnormal amount of vascular growth factor, which in turn stimulates angiogenesis, proliferation, and progression.
Photo 4 requires special attention because it shows a rare type of BCC, its scleroderma-like form. Only the abnormal vascular network gives the tumor away. The appearance of this tumor confuses even some doctors. The patient, not seeing something threatening and dangerous in the appearance of the skin, doesn't consult a doctor for a long time and lets the tumor progress in an excessive way. If such skin lesions are detected, especially on the nose or eyelid, you should immediately contact a specialist for diagnosis.
Photo 4

In photo 5, the skin of the back of the nose shows the beginning of the growth of a superficial form of BCC. The name "superficial" should not mislead readers. Superficial BCC proliferates not only radially, but can have invasive growth at a later stage of development.
 Photo5
Photo5
Photo 6 shows an image of a scalp, two scars after past cryotherapy, one of which shows signs of BCC recurrence. First of all, it should be understood that the probability of recurrence depends on many factors, and the probability is high, depending on the method of treatment and the size of the tumor. A BCC tumor, even of a very small size, first of all stimulates abnormal vascular growth. The structure of these vessels is also abnormal and incomplete, so they are very easily traumatized, "brittle", and ruptured. If the treated scar, after 6 months, suddenly begins to show faint redness and some bleeding, this can be a direct indication of scar recurrence.
Photo6 
Photo 7 can serve as an illustrative example of how in one area there can be several macro and micro formations of skin lesions, two of which (area 1 and 2) are visualized, and the bottom two (area 3 and 4) may remain completely unnoticed, not only by patients but also by doctors.

Photo 7
1. Easily visible and diagnosable tumor mass (BCC). By all external symptoms (nacreous papules, scab with signs of ulceration, presence of many threadlike vessels).The tumor differs radically from the surrounding healthy skin, indicating that it has achieved low differentiation, intracellular mutations and is prone to unceasing malignant progression.
2. An area and region of skin that has a high tumorigenic potential. In fact, it is a proliferating BCC tumor (active growth of atypical cells, abnormal angiogenesis (vascular growth)), but affecting and growing so far only in the upper layers of the epidermis without invading the dermis.
3. It is a small spot, completely unremarkable and capable of escaping every eye. But when you look very closely, you can see not only redness, but also the beginning of the formation of elevated skin scales (scab), which indicates the beginning of abnormal proliferation, which corresponds to the presence of atypical cells. The cells of this micro-site have a slow growth, medium patent to proliferation, since they have not yet accumulated enough cell mutations and have not yet completely lost cell differentiation (close to the phenotype of healthy tissue, cell formation and maturation, relative fullness of the genetic profile) and the ability to undergo the regulatory influence of the surrounding healthy skin cells. In comparison, tumor cells with low differentiation, as in the skin area (1), are completely autonomous, aggressive and do not experience any external inhibitory influence. The cells of skin area (3) continue to divide slowly, transform (mutate) and acquire a more malignant histological profile.
Very often, such subtle but pathological areas are overlooked or not taken seriously and ignored without treatment. Subsequently, for example, after surgical treatment of tumors 1 and 2, the forming scar usually gives rise to proliferation of slowly growing cells with tumor patency (area 3) not removed nearby, after about 12 to 36 months. If site 3 is further exposed to regular insolation, progression can be accelerated twofold or more.
4. An even less conspicuous area of the skin. This redness on the skin is barely noticeable and suspicious. As a rule, it does not stop even an attentive glance. The signs and fact of cellular atypia are there, but they are at the very beginning of their development and proliferation. One should pay attention to chaotically branched redness on the skin and formation of noticeable thread-like microvessels in this limited area, on the background of clean, contrasting with site 4 surrounding healthy tissue. When area 4, reaches a degree of malignant progression similar to area 1, it is still difficult to predict. Usually, it can take at least 2 to 10 years. But if there is or has been (already treated) a history of malignancy localized on the face, as in photo 7, the time when progression manifests may be shorter.
Since areas of skin 3 and 4 have minimal, initial and superficial development, they are easy to treat and prevent, but it must be timely, namely preventive.
Photo 8

Photo 8 shows a typical pigmented basal cell cancer. It differs from the other types only in the concentration of melanin in the malignant cells, which results in its dark color. This type of tumor usually occurs in brunettes, whose melanocytes tend to produce a high level of eumelanin under some kind of stimulation. It should be kept in mind that when such a tumor is detected, an urgent differential diagnosis is necessary in order to hastily verify the diagnosis, because melanoma has a similar external symptomatology and requires a biopsy.
Photo 9 shows the right side of the nose. A spontaneous ulcer that does not regenerate over a long period of time should raise the suspicion of a BCC diagnosis. In this case, the telangiectasia (many thread-like dilated blood vessels on the surface of the skin) is not primarily tumor related. However, excessive insolation in the past could be one of the reasons for their occurrence. If BCC at such a small size shows ulceration, this can be a sign of tumor tendency to invasive growth at the very beginning of its pathological development. There is a direct correlation between the depth of tumor invasion and the probability and frequency of its recurrence. A tumor that erupts in the early stages of development already tends to invasive vertical growth in the tissue, which can greatly complicate therapy.
Photo 9

Photo 10 shows superficial basal cell carcinoma on the upper lip. An emergency biopsy is mandatory for similar skin growths because of the similarity of these external features to squamous cell skin cancer.
Photo 10

BCC, it is a malignant tumor that metastasizes very rarely, giving people some time to make leisurely decisions, get diagnosed, and see a doctor or set of doctors. But those who have signs of a malignant tumor on the nose (especially), eyelid, ear, scalp, should remember that their time is limited and delay may be fraught with consequences, at least serious cosmetic defects. Therefore, it is recommended to immediately diagnose a specialist and begin treatment.
ACTINIC KERATOSIS AND SQUAMOUS CELL SKIN CANCER
Clinically, squamous cell skin cancer (SCC) usually presents as a single focus with conventionally circumscribed borders, irregular elevations on the tumor periphery over the rest of the skin surface, which are important and obvious signs that distinguish this malignancy from actinic keratosis. The tumor is usually localized in open areas of the skin. In 75% of cases, the face (nose, periorbital areas, auricles, temporal area, forehead) and hands are affected. The metastatic potential of this tumor reaches 20%. The task of the reader is to learn to identify and distinguish SCC tumors from actinic keratoses timely and independently. Timely see and detect the beginning of transformation, malignization of actinic keratosis into squamous cell skin cancer. Contact the specialists immediately!

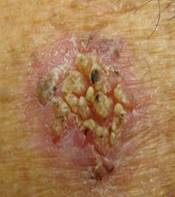

Photo 11 Photo 12 Photo 13
A high degree of cancer awareness is appropriate for people who have already been diagnosed with actinic keratoses (AK) or who have suddenly discovered a mass on the skin that has common features and similarities with AK. However, in order to avoid a constant worrying about it turning into an aggravating cancer phobia, the reader only needs to be attentive and form a correct idea of what the symptomatic features and external distinguishing features between AK and SCC are. Clinicians have had numerous observations of AK passing through all stages of development maligning into SCC. But, there are enough other examples of skin cells adopting their malignant histological profile at the earliest stages of tumor formation, bypassing the hyperkeratinization stages.
As for the period of malignant transformation of AK into SCC, it is worth noting at once an important distinctive aspect. Uniformly and at the same time scatteringly forming hyperkeratosis on the skin, even in excessive amounts, usually serves as an indicator that the cells still retain relatively high differentiation (phenotype-genetic profile of the cell, still close to the phenotype of a healthy cell), and, still not a malignant tumor. And what is remarkable is that as the mutations (genetic transformations) accumulate, the cell steadily becomes malignant and progresses, the tumor significantly or completely loses over-activity of keratogenesis and horny layer formation. Accordingly, the more keratinocytes are replaced by malignant cells, the less horny scales are formed on the skin, as the evolution of the malignant cell begins to acquire a different vector of development and begins to take both an external and histologically quite different appearance.
For example. Photo 11 shows an actively progressing actinic keratosis. Absence of clear boundaries of process spreading, moreover, such pronounced keratinization, keratosis formation in different degree, but all over the skin lesion area, indicates absence of malignant transformation. Requires treatment.
In photo 12, we should note not typical changes of keratinization with formation of isolated large scab grains, concentrated in the center, with loss of keratinization around the formation. Such changes may indicate the onset of malignant transformation or at least the emerged malignant potential. Requires serious attention and referral to a specialist. Photo 13 shows a typical picture of one stage of a tumor mass, with complete loss and inability to keratinize at the periphery of the tumor, with temporary preservation of the scab in the center of the mass (as the tumor develops, the residual keratinization will be replaced by the erupting mass of the tumor). The detection of such a mass on the skin requires urgent and immediate medical attention!
Photos 14 and 15 show two different cases of the same type of malignant progression. The fact that this type of SCC was not preceded by long-term actinic keratosis requires attention. Photo 14 shows the onset of tumor development (superficial, with a low probability of metastasis). There is an outward resemblance to the superficial type of BCC, so a timely differential diagnosis (biopsy) is necessary. Photo 15 shows the radial growth stage of SCC progressing to an aggressive proliferation stage. The probability of metastasis in this case is very high. The tumor progression to this stage can be due to a number of reasons. Not infrequently, this is due to the localization of the tumor, which is difficult to visualize. This is especially true for single people of retirement age. If such a mass on the skin is detected, it requires urgent consultation with a doctor!
Photo 14 Photo 15


Photo 16 (Keratoacanthoma) and 17 (SCC) are two very similar looking tumors. Yes, most keratoacanthomas have a benign course, and transformation into SCC is rare, but the possibility always remains. It should be noted that most "non-hazardous" keratoacanthomas grow quickly and regress within about 6 months. Difficulties are presented by keratoacanthomas, which grow slowly and for more than one year. Such tumors should be considered potentially dangerous. In such cases, diagnosis and treatment are necessary.
Photo 16 Photo 17


In this article, we present pictures with large malignant neoplasms for visual demonstration and convenience of visual perception. The challenge for the reader is to learn to identify independently at the very beginning of their malignant origin, when they are small, on the background of actinic keratosis, in hard-to-reach places, on the scalp.
MELANOMA
Unfortunately, we have to agree with those doctors and colleagues who call melanoma the queen of all malignancies. The difficulty seems to be in everything, in timely early diagnosis, in the development and clinical study of drug forms, and in the search for a complete understanding of the pathogenesis of this so rapid and ruthless pathology. At the moment, self-monitoring and self-diagnosis in this disease, is the most important, with the purpose of early detection of pathology !
Photo 18 Photo 19 Photo 20



Photo 18 shows an advanced melanoma localized between the toes. The plantar part of the feet, the crease of the toes, is one of those problematic locations where dysplastic nevi can be located. The area between the toes is not exposed to insolation, but is subject to mechanical friction and irritation, which may be enough to transform this type of nevus into a melanoma. Preventive screening of these areas is mandatory.
Photo 19 The photo shows a dysplastic nevus. This nevus has a direct relation to the development of melanoma, and as a precursor of melanoma, this type of nevus is subject to the most serious approach in diagnosis. Based on many years of observations, it was found that the degeneration of nevus dysplastic type in a malignant tumor is one hundred percent likely, and therefore doctors are trying to learn as much as possible about the causes of its occurrence. Dysplastic nevus, as a spot of pigmented education, has irregular shapes and outlines in the form of blurred borders. The color of this type of nevus varies in the range of light brown and purple-brown shades of color. Locations of such nevus are usually areas of the body that are hidden from view (chest or buttocks, finger folds, back). Although there is no guarantee that such a disease will not be in any other place. Among other things, such a formation is famous for its "family" in terms of the number of stays on the skin, where the body of one person sometimes has as many as hundreds. Prophylactic inspection of the above mentioned areas is extremely important. If suspicious nevi are found, an immediate visit to the doctor is necessary!
Photo 20 shows a pigmentless melanoma. If a similar or suspicious nevus appears spontaneously, see your physician immediately!
Photo 21 Photo 22


Photos 21 and 22 show a lentigo, an age-related skin pigmentation that can also transform into a melanoma. Photo 21 shows a lentigo of a healthy person. In photo 22, a melanoma has formed on the periphery of the upper part of the lentigenosis.
Photo 23 Photo 24 Photo 25


Photos 23 and 24 show melanoma on the back of the shin. Atypical irregular form, irregular accumulation of melanin, surrounded by small melanocytic nevi. Photo 25 shows a melanocytic nevus surrounded by a light, hypopigmented rim (Seton's nevus), usually not threatening. However, if such a nevus is detected, a differential diagnosis by a physician is necessary, because in some cases, the human immune system may respond to a melanoma manifestation with a hypopigmented halo.
Photo 26 Photo 27


Photo 26 shows benign keratomas, or single, but not infrequently multiple. The edges are flat, regular in shape.
Compared to photo 27, melanoma. Usually a single mass. The edges are blurred, the shape is not uniform, and the color is darker.
Photo 28 Photo 29


Photo 28 shows a nail hematoma. Photo 29 shows a melanoma. It is important to remember that if the appearance of a pigmented formation on the nail, not preceded by an injury, it should be regarded as a dangerous signal and a reason to see a doctor immediately. A normal nail hematoma always has "blurred" edges. Note that while melanoma is in its initial development, has superficial growth, it most often develops linearly with clearly delineated borders as in photo 29.
It is difficult to overestimate the importance of self-examination, regularly performed alone or with the participation and help of an additional pair of eyes. If you have a suspicious melanocytic nevus, for example, between your toes, only you will know, and you should tell your doctor about this finding, because most doctors will not even think of checking every crease between your toes, carefully checking your scalp and moving every strand of hair in their hands. No, it is up to you, and not without the help of your loved ones, to point out this or that finding to the doctor.