 30.11.2020
30.11.2020
The mammary glands are made up of three main types of tissue: adipose, connective and glandular. Breast cancer (BC) is the name given to malignant tumors of the breast that develop specifically from the cells of glandular tissue. Contrary to popular belief, breast cancer affects both women and men, but women are about 100 times more likely to get it.

Breast cancer develops just like any other malignant tumor. One or more glandular tissue cells, as a result of a mutation that has occurred in them, begin to divide abnormally quickly. They form a tumor that can sprout into neighboring tissues and create secondary tumor foci-metastases.
Mutations that lead to breast cancer can be inherited or acquired.
Common hereditary genetic causes are mutations in the BRCA1 and BRCA2 genes. BRCA1 mutation carriers have a 55-65% risk of getting breast cancer, while BRCA2 carriers have a 45% risk. These genetic defects are inherited from parents to children and cause cancer in about 15% of cases.
Much more often, breast cancer is due to acquired mutations: they appear in the cells of the gland and are not inherited. For example, in 20% of cases the number of copies of a gene is increased, encoding HER2, a receptor protein that resides on the surface of cells and stimulates their proliferation.
Types of breast cancer are divided into two groups: ductal and glandular. Ductal cancer is more common. It can be intraepithelial (in situ) and invasive. Intraductal breast cancer has a more favorable prognosis, it rarely gives metastases and is cured in 98% of cases. The invasive variant of a tumor is prone to uncontrolled growth and generalization of process. Glandular cancer can be lobular (invasive lobular carcinoma) or grow from other glandular tissue cells. Lobular cancer is often characterized by multicenter growth. The rate of increase in the size and terms of metastasis of the forms of nodular breast cancer depend on the degree of differentiation of a tumor of the breast.
Risk factors associated with external influences and lifestyle
Low level of physical activity. Scientists are finding increasing evidence that it's a factor that puts you at higher risk for breast cancer. At the same time, it is well known that regular physical activity helps to reduce risk, especially in postmenopause.
It is not known how physical activity contributes to cancer prevention. It is thought to be through normalization of weight, metabolic processes, hormonal background, and reduction of inflammation in the body. There are no specific recommendations about the duration and regularity of exercise, but many experts say that even exercising for two hours a week will be beneficial.
Overweight and obesity. Being overweight as a risk factor for breast cancer starts to work hardest in postmenopause. In women of reproductive age, estrogen hormones are produced in the ovaries. After menopause, this function is mainly taken over by adipose tissue. If there is a lot of fat in the body, more hormones will be produced. And this can contribute to the growth of a malignant tumor. Also, overweight people have higher insulin levels.
However, the link between excess body weight and the risk of developing breast cancer is not so simple. In contrast, studies show that pre-menopausal women who are obese are somewhat less likely to develop a malignancy. Also, the amount of adipose tissue in the body is differentially associated with different types of breast cancer:
- being overweight after menopause most strongly increases the risk of developing hormone-positive malignancies;
- some studies show that extra pounds gained before menopause increase the risk of developing triple-negative cancers.
The risk increases in parallel with how often and in what amounts a woman drinks alcohol:
- drinking 14 grams of ethyl alcohol per day increases the risk by 7-10% compared to non-drinkers;
- At 28-42 grams of ethanol per day, the risk increases by 20%.
- Age at first birth and number of pregnancies. In general, women who first gave birth after age 30 have a slightly higher risk of developing breast cancer. And first pregnancy at a young age and multiple pregnancies are associated with a lower risk.
- Lack of breastfeeding. Studies show that breastfeeding somewhat reduces the risks, especially if it lasts more than a year. The mechanism for this protective effect is not understood. This may be due to the fact that the total number of menstrual cycles during a lifetime is reduced by prolonged breastfeeding.
- Breast implants do not increase the risk of breast cancer, but anaplastic large cell lymphoma can develop in the scar tissue near them. These tumors most often occur with textured implants with rough surfaces.
- As for contraception and hormone replacement therapy, we cannot share the worldwide prevailing view that hormones play a minor role in cancer development or are all safe (We will publish the results of our research and studies screening our colleagues on this topic in a while)
Risk factors that cannot be influenced
Female gender is the most obvious risk factor for developing breast cancer. Men also have the disease, but much less frequently.
-Age. Over time, mutations accumulate in body cells, including those associated with malignancy. Breast cancer is most often diagnosed in women over 55 years old.
-Hereditary mutations. It is believed that 5-10% of malignant breast tumors are hereditary - they arise from mutations present in the cells of the body since birth.
The most common hereditary mutations associated with breast cancer are changes in the BRCA1 and BRCA2 genes. Normally, the products of these genes are involved in the repair (repair) of damaged DNA. If they do not work properly, the DNA is not "repaired", more mutations accumulate in the cells, and these cells can become cancerous. Carriers of mutations in the BRCA1 or BRCA2 genes have a 70% risk of developing breast cancer by age 80. In addition, there is an increased risk of developing ovarian cancer and some other malignant tumors.
Hereditary mutations in other genes can also lead to breast cancer:
-TP53. The protein encoded by this gene (p53) is called the "guardian of the genome. It stops the growth of cells with damaged DNA and forces them to commit "suicide". Hereditary mutations in the TP53 gene are diagnosed with Li-Fraumeni syndrome. Such people have an increased risk of developing breast cancer, malignant brain tumors, leukemia, and sarcomas.
- ATM. The product protein of this gene is involved in repairing damaged DNA or killing the cell if "repair" is not possible. In hereditary mutations in ATM, ataxia-teleangiectasia develops. Breast cancer is common in some families with these mutations.
- PTEN is a gene that is involved in the regulation of cell growth, and hereditary mutations in it develop Cowden syndrome. This rare disease increases the risk of developing some benign and malignant tumors.
- CHEK2 encodes a protein that is involved in DNA repair.
- STK11 is a gene in which hereditary mutations cause Peutz-Yeghers syndrome. These patients have pigmented spots in the mouth and lips, polyps in the digestive tract and urinary tract, and an increased risk of developing some malignant tumors.
- CDH1. Hereditary mutations in this gene develop a rare malignancy, hereditary diffuse gastric cancer. Women also have an increased risk of developing breast cancer.
- PALB2. The protein that encodes this gene works in conjunction with the protein encoded by the BRCA2 gene. Therefore, mutations in it also increase the likelihood of malignancies in the breast.
- Family history. Approximately 15% of women with malignant tumors in the breast have close relatives with the same diagnosis. If your mother, sister, or daughter is diagnosed with breast cancer, your risks are almost doubled, and if two close relatives are diagnosed at once, three times as high.
- Personal history. If a woman has already been diagnosed with breast cancer, the risk of malignancy in a second breast or other organs is slightly increased.
-Race and ethnicity. In general, breast cancer is more common in Caucasian women than in black women, but in the latter, such tumors are more frequently diagnosed before age 45 and have a higher mortality rate. Both the prevalence and mortality rates of breast cancer are lower among Asian women.
-Height. For unknown reasons, breast cancer is somewhat more common in taller women. Early nutritional habits, hormonal background, and heredity may all play a role.
Peculiarities of the menstrual cycle. The risk of developing breast cancer is slightly increased if:
- her first period came before age 12;
- menopause occurred after 55 years of age.
Radiation therapy. The risk of breast cancer is increased in women who underwent breast irradiation when they were young, in their teens, when breast tissue was still forming. For women over the age of 40, these risks are absent.
Xenoestrogens and phytoestrogens are considered endocrine disrupting chemicals. This means that these compounds affect the synthesis, secretion, transport, metabolism, binding or excretion of natural hormones, which are present in the human body and are responsible for homeostasis, reproduction and development. It has now been shown that their mechanism of action is much broader than originally thought. In particular, xenoestrogens, in addition to their interaction with estrogen receptors, can bind nonnuclear steroid hormone receptors (e.g., membrane ER), nonsteroid receptors (e.g., serotonin, dopamine norepinephrine receptors), orphan receptors (e.g., aryl hydrocarbon receptor) and affect the enzymatic pathways involved in steroid hormone biosynthesis . Let's take a closer look at all three groups of hormones.
The most common xenoestrogens and their effects on reproductive function and human health.
Xenoestrogens are synthetic environmental compounds that have similar activity to endogenous estrogens and mimic the properties of these hormones. They can actively interact with the cell by binding to the estrogen receptor (ER) on its surface, triggering a whole cascade of reactions, often completely unpredictable.
Diethylstilbestrol, 4,4'-dichlorodiphenyl-trichloroethane (DDT), bisphenol A are the most studied molecules by mechanism of action, although the xenoestrogens group is not limited to them.
4,4'-dichlorodiphenyl-trichloroethane (DDT) is an organochlorine pesticide that interacts with ER -α and ER -β . In 1939 Swiss chemist P. Müller discovered its insecticidal properties, for which he received the Nobel Prize in medicine.
In 1950-1980s. In 1950-1980 about 400 thousand tons of DDT were used annually all over the world. In 1972 it was banned almost everywhere in the world, with the exception of a few countries.
DDT is highly resistant to degradation, cumulates in the food chain and accumulates in human adipose tissue. To date, it has been detected in the breast milk of most lactating women. Today, it is virtually impossible to find living organisms on the planet that do not contain DDT. As early as the mid-1960s, DDT was found in the liver of penguins in the Antarctic, very far from where the chemical was used. Epidemiological studies in humans have linked DDT use to sperm quality disorders, menstrual irregularities, and decreased lactation time. A prospective study of a group of Chinese female workers found an association between DDT levels before conception and subsequent risk of early pregnancy loss. Exposure to DDT is a risk factor for preterm birth and low birth weight. The effect of DDT on breast cancer risk is still debated.
Bisphenol A (BPA) is a monomer used to make polycarbonate plastics and epoxy resins. Polycarbonate plastics are widely used in consumer products such as water bottles, baby bottles, toys, some medical devices, etc. BPA is also used in epoxy resins for internal coating of canning jars, it is a part of some dental sealants and composites. Almost everyone in the developed world is now exposed to BPA. According to a study by Eun-Ji Kim and Dongho Lee, BPA was detected in the urine of 97.3% of Koreans surveyed. In population studies by other colleagues, BPA was detected in 91% of the Canadian population, in 93% of the U.S. population, and in 92% of the German population. The primary route of exposure is oral, as BPA can migrate into food from beverage and food containers. Because BPA is a weak estrogen, it was long thought that doses to humans at home had no significant effect on health, but it was then found that bisphenol can bind to membrane ER and initiate a rapid cellular response even at low doses.
Concerns about human health effects are largely due to a number of animal studies that have shown that bisphenol can affect biological systems even at low doses. For example, in animals, exposure to low doses of bisphenol during critical developmental periods can lead to changes in behavior, brain function, and breast cancer.
Ways to reduce bisphenol exposure:
- Do not put polycarbonate plastic containers with food in the microwave;
- Avoid using containers that are labeled with the number 7 on the bottom, as some may contain bisphenol A;
- reduce the use of canned foods;
- Do not use baby bottles containing bisphenol A;
- If possible, use glass, china, stainless steel, or safe types of plastic for hot foods or liquids.
The effect of lifestyle was demonstrated in a study involving 77 college students who experienced a 2/3 increase in urinary BPA concentrations after students drank water from a bottle containing BPA in polycarbonate plastic for 1 week.
Phytoestrogens and their influence on reproductive function and women's health.
Phytoestrogens are a vast group of molecules of plant origin that have estrogen-like and anti-estrogenic properties. They are chemical substances that have a structure similar to natural estrogens and can bind to both ER-α and ER-β, but are characterized by greater affinity for ER-β. In humans, phytoestrogens behave in two ways: as agonists and antagonists at the same time. Phytoestrogens can be classified as flavonoids, coumestanes and lignans; each group includes a large number of molecules with different degrees of estrogenic activity, which makes them difficult to study. Flavonoids are one of the most common classes of phytoestrogens because they are most commonly found in food sources. Most studies have focused on resveratrol, quercetin, daidzein, and genistein because they are among the most commonly consumed groups of phytoestrogens. A feature of some phytoestrogens is also that the formation of active molecules requires the presence of specific gut microflora, which is not present in everyone.
Exposure occurs mainly through the consumption of beverages and foods containing fruits and vegetables, herbs and especially - soy products, which are characterized by a high concentration of phytoestrogens . Soy protein is added to many meat products and confectionery, and soy-based baby foods now make up to 1/3 of the developed markets. As a result, infants who received soy-based formula have circulating phytoestrogens concentrations of about 1,000 ng/mL, which is 13,000 to 22,000 times higher than their own endogenous estrogen levels, 50 to 100 times higher than estradiol levels in pregnant women, and up to 3,000 times higher than estradiol levels at ovulation. Traditionally the intake of isoflavones in Koreans, Japanese, Chinese reaches 50 mg/kg body weight per day, but also in Europeans and Americans who lead a vegetarian lifestyle or use dietary supplements, the intake of phytoestrogens can reach the same level as in Asians, or even higher.
The incidence of vasomotor menopausal manifestations is higher in Western countries (70-80% of women) compared to Asian countries (10-20%). This observation has led to the popularization of the idea that soy-based phytoestrogens may alleviate the menopausal period. Unfortunately, in a number of studies, the use of phytoestrogens for this purpose had no or minimal clinical effect compared to placebo. A 2007 Cochrane systematic review of 30 randomized controlled trials (RCT) failed to confirm the efficacy of using dietary estrogens compared to placebo. At the same time, a large number of studies have been published confirming the efficacy of a number of phytoestrogens in the treatment of vasomotor symptoms, leading the North American Menopause Association (NAMA) to recognize the feasibility of isoflavones as a starter therapy for vasomotor disorders.
In 2008, a meta-analysis of 8 RCT showed that increased soy consumption led to a reduced risk of breast cancer in a population of Asian women. It found that 10 mg of soy per day was sufficient to reduce the risk of breast cancer by 12%. These findings were not confirmed for Caucasian women, but the average daily dose of isoflavones in this group was significantly lower (up to 1 mg per day). Ironically, another meta-analysis of 18 studies published between 1978 and 2004 found a protective effect of soy in the premenopause in Caucasian women, but not in Asian women.
In a study by V. Beck et al. showed by competitive radioligand binding that phytoestrogens bind to androgen receptors (AR). Isoflavones, biocanin A and genistein, suppress the expression of genes that regulate AR activity, which may be manifested by decreased levels of dihydrotestosterone involved in the production of prostate-specific antigen (PSA) in breast and prostate cancer. The molecular mechanism of the anti-androgenic effect of isoflavones on androgen-regulated AR gene expression is not yet clear. Perhaps one pathway is the inhibition of AR or androgen-controlled genes, receptor blockade, or a combination of the two. It is likely that the ability of some isoflavones to block PSA production will be the subject of further research. Isoflavones have been shown to affect not only ER and AR, but also progesterone receptors (PR). The specific effect of flavonoids on the ER or PR depends on the position of the B ring with respect to the flavonoid core. Substances with progesterone and androgenic activity are flavones or flavonoids and differ from isoflavones in their lower affinity for the ER.
It was also shown by the competitive binding method that the isoflavone of red clover extract can also bind to PR, acting as a weak agonist. In a comparative study of various plant extracts, red clover extract preparations were found to bind more firmly to PR than soybean preparations. Isoflavones are believed to be weak ER -α agonists and strong ER -β agonists. This fact and the different distribution of both ERs may explain the tissue specificity of phytoestrogens. J. An et al. attempted to explain the molecular mechanisms of ER -β isoflavones mediated response of target genes.
They found that the direction of transcription induced by isoflavones differs from that triggered by estrogens. Moreover, the binding of isoflavones determined by competitive radioligand binding is stronger with ER-β than with ER-α .
Phytoestrogens also affect various enzymes involved in steroid hormone metabolism. Aromatase, the enzyme that converts androstenedione to estrone and testosterone to estradiol, is inhibited by phytoestrogens. Le Bail et al. found that aromatase was less inhibited by phytoestrogens than 17-β hydroxysteroid dehydrogenase (17-HSD) or anti-3β-hydroxysteroid dehydrogenase isomerase (3β-HSD). Estrogen-positive, estrogen-dependent forms of the disease are found in 60% of patients with breast cancer. When aromatase is inhibited, endogenous estrogen production is reduced. Inhibition by phytoestrogens may account for the protective effect against the development of breast cancer in populations of women who eat foods high in isoflavones. A. Krazeisen et al. studied the inhibitory effect of phytoestrogens on 17-β HSD. S. Makela et al., using three different breast cancer cell lines, found effects of phytoestrogens on 17β-HSD type 1, which converts estrone to estradiol. Isoflavones affect a number of key enzymes of steroid metabolism and consequently reduce the level of local hormone activity in the relevant tissues. This is likely the biochemical basis for the protective effects of a diet rich in isoflavones and inhibiting the development of breast cancer in the first place. There is evidence to support the concept that phytoestrogens can influence the sensitivity of breast cancer cells to vitamin D analogues and prevent their proliferation.
The evidence from in vitro experimental studies varies. While there is no evidence that isoflavones affect breast cancer, there is also evidence of adverse effects. The debate about breast cancer risk in relation to isoflavones continues.
For example, it is thought that isoflavones have the potential to prevent breast cancer, but it is unclear whether they have an estrogen-like or anti-estrogenic effect on breast tissue.
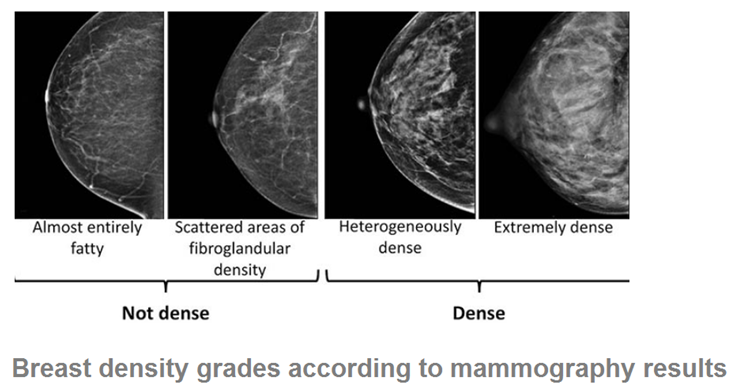
Mammographic density is known to be a prognostic risk factor for breast cancer. A double-blind, randomized, placebo-controlled study (performed by two groups of investigators) determined the effect of isoflavones extracted from red clover on mammographic density. Mammographic density before treatment was 68.1±14.4 and 61.5±18.8%. According to the data obtained by the scientists in the first group in women taking isoflavones and placebo, mammographic density decreased by 22% and 18%, respectively. In 78% of cases, mammographic density did not change and only 2% increased. A second group of researchers reached a similar conclusion.
One of the isoflavones in red clover extract, genistein, reduces the activity of CYP24 enzyme responsible for the breakdown of a metabolite of vitamin D (25-dihydroxyvitamin D ), which has antimitotic effects and can probably contribute to cancer prevention.
It is known that high serum concentrations of insulin-like growth factor-1 (IGF-1) during menopause can increase the risk of breast cancer. Results of a randomized, placebo-controlled, cross-over study showed a decrease in IGF-1 concentrations after 1 month of taking 86 mg/day of red clover extract compared to placebo.
THE ROLE OF PROLACTIN
Studies were conducted to find out a possible procancerogenic role of prolactin.
All patients were between 50 and 73 years of age (median age was 62.5 years). All patients were in menopause from 5 to 25 years. By histological structure all malignant neoplasms of the breast and endometrium were adenocarcinomas of predominantly moderate degree of differentiation.
We found out that level of prolactin was elevated in all tissue samples of breast tumors studied, however the degree of increase of the hormone content was different. Thus, in breast malignant tumor tissue of primary independent process the level of prolactin was increased only by 12.2% in comparison with intact tissue, while in tumor tissue of combined breast cancer and uterine myoma the increase was 61%. It is interesting that in the tissue of a benign tumor (nodular form of cystic fibrosis) the prolactin content exceeded the normative values by 23.1%, i.e. was higher than that in the primary independent malignant process.
Our results are in agreement with the data described in the literature on the increased level of prolactin in cancer patients and, in particular, in the breast cancer tissue. The fact of hyperprolactinemia in patients with autoimmune diseases suggested that prolactin has immunoregulatory properties. It has now been established that prolactin acts as a hormone and cytokine capable of influencing cell metabolism by enhancing cell growth and division. With regard to the breast, it is believed that adipocytes are a potential source of relatively high concentrations of prolactin at the site of tumor formation, providing the main links in the pathogenesis of cancer of this organ. This position is also confirmed by Clevengeretal (1995), who showed that one of the mechanisms of tumor progression in the breast is a significant change in the level of prolactin and expression of receptors to it. A direct correlation between the number of prolactin and estrogen receptors was also found
As a result of examining the level of progesterone in the tissue samples we studied, we found that during the independent development of tumors in the mammary gland, the content of progesterone was reduced only in the breast cancer tissue by 37.1%, while in the tissue of a benign tumor (nodular form of FCD) no changes in the hormone level were found in comparison with the intact tissue. One could find a 1.9-fold decrease of progesterone content in the endometrial cancer tissue compared to the corresponding control samples, while in the uterine myoma tissue, its level did not differ from the normative values during this variant of development. At the same time, at the combination of breast cancer and uterine myoma both tissue samples showed 1.9 and 2.2-fold decrease of the hormone level respectively in comparison with intact breast tissue.
It is possible to summarize and say that in spite of a lot of discoveries and the results of the research in the field of physiology and molecular biology, we are only at the beginning of the way of knowledge of this pathology, the course of many microprocesses in macroorganism.